I am a health professional
Polio Survivors Network was made aware in the late 1990s that Colleges of Medicine had been reducing the facts taught about polio. This was due to the polio vaccine success (12th April 1955) which reduced the number of people being infected by one of three polio viruses.
Some health professionals told us that polio was not mentioned during their training, others remember having a half hour lecture with leprosy and seeing photos of withered limbs and patients in iron lungs.
Polio Survivors Network research has picked up three possibly missed issues:
- The high level of recovery many polio survivors reached
- How questions are asked by health professionals and how polio survivors answer
- Often a single action manual muscle test is used
1. Many members have been in the armed forces, police, professional sportsmen and women, and had other physical occupations report being told ‘you must have had a mild case’ when in fact they had paralysis in at least one limb and some spent some weeks in iron lungs. The following slide is taken from the PowerPoint Presentation – Information from a Polio Survivors Perspective – and used by the author for over 20 years.
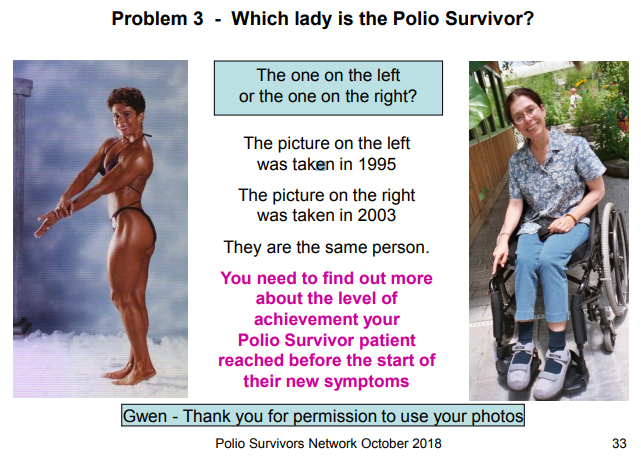
People who had polio and are experiencing new symptoms, after years of stable functioning, need to be assessed by medical professionals who are knowledgeable and experienced in the effects of the original polio infection, level of recovery, and post-polio. Unfortunately for health professionals, there are no tests to confirm post-polio, tests can only rule out other conditions, it is a diagnosis of exclusion.
Assessing a polio survivor, especially one who has not long learned about this later stage to having had polio, is not easy. Polio survivors are reported to be strong-willed, determined, and even pig-headed people who have got on with their lives achieving as highly as they can despite their level of polio damage. The last place a polio survivor with new medical problems wants to be is in a doctor’s office. Nearly all polio survivors I have met, fit this category including me. Many have blocked or suppressed memories and emotional responses to sights, smells and sounds from the past. One member only a year ago asked why the nurses in the UK did not wear black. Further questioning elicited the fact that he had been in a catholic hospital when he was having his surgeries aged 5 to 8 and the nurses were nuns first. Not once in 60 years had he made the connection.
It is therefore important to note that to be in your office polio survivors are likely to have been experiencing symptoms over a long time – months and even years – and they are reluctant to admit that actions of daily living are becoming harder. As actions of daily living become more difficult they adapt how they do an action and it becomes their new norm. Often they do not notice or don’t want to accept that this is happening. It is very hard to change from our childhood ‘Use it or lose it’ mentality. So many of us will respond to advice to pace and rest or start using aids and assistive devices with ‘But I am not there yet’.
2. You can ask five polio survivors ‘Can you get up a flight of stairs? All will answer ‘Yes’ and be proud that they can do this action. However, if you had asked ‘How do you get up a flight of stairs? The responses would be, [a] walks up, [b] walks up right leg first, [c] does the same but stops half way to rest, [d] also has to use the bannister rail to pull themselves up and [e] sits on the stairs and goes up backwards one step at a time pushing up with their arms. Help us tell it like it really is by asking us ’How do we do x, y or z?’
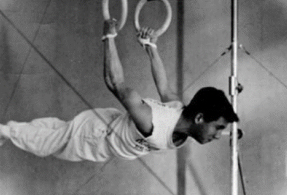
Take this patient as an example… He was born in 1946 and grew up and went to school in New York. He made the Gymnastics Team at College. At the University of Tucson in Arizona, he gained a Bachelor’s Degree in English Literature, a Masters Degree in Special Education and a Bachelors in Nursing. He worked as a private school teacher in English and Science then as a Critical Care Registered Nurse in Cardiac Surgery.

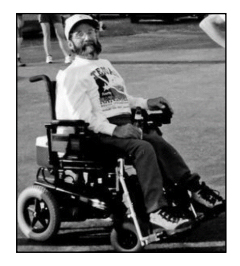
Meet Charlie
On the left, he is 10 years of age.
On the right, he is 53 years of age.
The photo above was when he was 19 in his college gymnastic team.
3. When assessment time is short and Single Action Manual Muscle Testing is used. This can be unreliable where weakness in muscles is not evident until a few repeats or some seconds later than the time available for testing. There can also be issues where the pattern of movement is not tested.
I spent seven years following a fall and new weakness and pain in my left arm with no corroboration of the reported symptoms. All muscle testing by consultants and physiotherapists failed to pick up any weaknesses. My prior diagnosis of paralytic polio was not in the equation. From 1988 to 1975 normal results for Single Action Manual Muscle Testing had been recorded on all medical reports. In 2004 when the asked for baseline assessment was being undertaken by a senior physiotherapist I asked ‘Why am I now scrambling eggs with elbow rotation?’ Specific examination found extremely weak supinators. Of possible interest is that in 1989 when receiving the results of my nerve conduction studies I was told they would operate on the ‘carpal tunnel syndrome’ in my right wrist. I refused as all the pain and weakness was in my left arm. Could the ‘carpal tunnel syndrome’ have been polio nerve damage?
We advise our members that the most important facts to give health professionals are relating the change in the way they are now having to do actions of daily living and ask why?
To assist polio survivors to ‘see’ the changes in black and white (although this is often a difficult experience for them) we suggest that they make up a file of information on their lives. To assist them with this we have formulated a Self Assessment Tool called ‘My Polio Life’. We do not advocate their bringing the whole file to the appointment but pick from it the important points relevant to this appointment and collate this on one sheet of paper. We suggest that they offer a copy to you if you wish. Some health professionals have welcomed this, written notes on it, and placed it in the patient’s file. Others have refused as they have their own procedures. We suggest that they provide a couple of photos to give you more information on their level of recovery.
Symptoms of Post-Polio Syndrome:
• Fatigue often overwhelming, both physical and mental
• Loss of muscle strength and/or use (often in muscles below the line of clinically evident weakness during original infection)
• Pain in muscles and joints
• Trouble breathing and/or swallowing
• Problems sleeping
• Intolerance of cold, causing muscle weakness and sometimes burning pain and/or discolouration in limbs1. A history of remote paralytic polio or findings on history, physical examination results, and laboratory studies compatible with polio virus damage of the central nervous system in earlier life.
2. A period where we recovered.
3. A stable period of functioning, from 10 to 50+ years.
4. New symptoms with no other explanation.
THERE ARE NO TESTS – IT IS A DIAGNOSIS OF EXCLUSION.
Please see our Helpful Resources page for information specifically aimed at healthcare professionals
